With the passage of Medicare in 1965, President Lyndon Johnson opined “No longer will illness crush and destroy the savings that [older Americans] have so carefully put away over a lifetime.” As the demographics of this country expand the pressures on our slowly growing economy, payment for an expensive illness response system may indeed crush many of us, especially those whose earnings have stagnated over the past three decades, which includes households with income in the bottom half of the nation’s distribution of income.
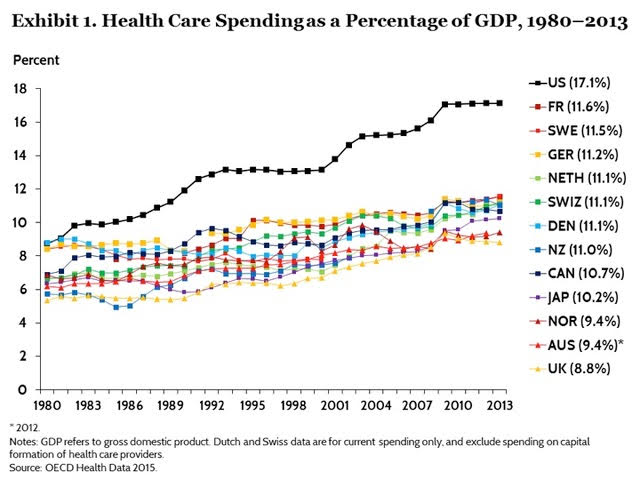
1. Expenditures on medical care have grown 2.5% more rapidly than GDP since the passage of Medicare and Medicaid in 1965 and 2% more rapidly since 2000. Recent projections suggest that we are likely to be spending 20% of our income on medical care related activities by 2025 (S. Keehan, Health Affairs, 2017). At present, we are approaching 18%; no other major country exceeds 12%. (See below graphic.) Clearly, this must stop at some point. The population might be willing to continue to give up other goods and services for more medical care if their collective health improved, but much evidence – for example, A. Case and A. Deaton (Brookings, 2015) and D. Cutler (The Quality Cure, 2014) – suggests that our vast expenditures on clinical services has not led to anything like proportionate increases in either life expectancy or improvement in health.
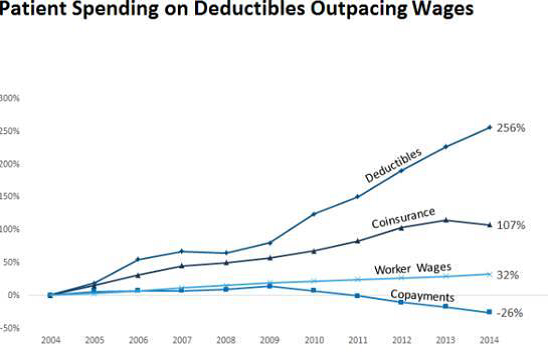
2. At the individual level, the lack of sustainability is even more clear. Between 2004 and 2014, as shown in the below graphic, the average level of deductibles grew by 256% while wages have only grown by 32%. This rise is especially burdensome on those covered by insurance but in the bottom quartile of wage earners. A recent study (B. Sherman et al., Health Affairs, 2017) suggests that workers in the lowest wage quartile have almost twice as many hospital admits, more than four times as many avoidable hospitalizations, and more than three times the number of emergency room visits as those in the top wage quartile; thus high deductibles impinge significantly on the modest incomes of those who earn low wages. Furthermore, the economic impact of a major injury or illness, in particular for people admitted to a hospital, can last for years through an increase in unpaid medical bills and potential bankruptcy as well as reduced household income (C, Dobkin et al., NBER, 2016).
3. The political sustainability of expanded Medicaid clearly must be questioned. Projections for increased national debt levels relative to income arise largely from three programs: Medicare, Medicaid, and Social Security. For example, the House of Representatives’ AHCA and the proposed Senate BCRA cut the funds for Medicaid over the next 10 years by more than $700 billion.
So what factors led medical care in the United States along such an unsustainable path? Many answers have been cited; this posting will address four pertinent ones.
1. The payment system for medical goods and services has been structured to benefit those (such as physicians, hospitals, insurers, and pharmaceutical firms) who provide both more and more intensive services. Despite recent legislative changes in Medicare payment policy (MACRA 2015), fee-for-service payment systems still dominate most markets; thus, costs continue to escalate and with them both insurance premiums and out-of-pocket expenses. To keep premium increases from exploding, higher deductibles have been the favored response in both the group and individual insurance marketplaces. Note the implications in point 2 above.
2. State and Federal tax exemptions and deductions exacerbate the above forces. The Congressional Budget Office (2016) estimates that employer sponsored insurance (ESI) exemptions alone will reduce Federal taxes collected by $268 billion (in 2016) and by over $3.6 trillion over the next 10 years. This swamps the cost of the Medicaid expansion under the ACA ($70 billion in 2016 and $856 billion over the next 10 years and subsidies for those who participate in the federally facilitated exchanges ($48 billion in 2016 and $919 billion over the next 10 years.) Furthermore, the vast majority of the ESI exemptions benefit those families with income in the top 20%.
3. Despite substantial evidence that resources devoted to the medical sector account for no more than a quarter of the improvements in health seen in the U.S. , the U.S. continues to devote a substantial majority of such resources to medical care with much smaller shares to the other determinants of health (individual behavior, socio-economic characteristics, and the physical environment.) Other countries, that achieve better outcomes, have a more balanced distribution of resources (E. Bradley and L. Taylor, The American Health Care Paradox, 2013) and superior health outcomes.
4. Increasing consolidation in both the provider and insurer markets have led to a lack of competition in the provision of health care and insurance services (M. Gaynor, Health Affairs, 2016). Furthermore, much of this increased market power has been the result of non-local organizations taking over the leadership from community-based organizations. As a result, existent health care systems, physician groups, and insurers tend to focus on revenue and market share objectives rather than on efficient delivery of an appropriate set of health services to serve community needs.
One thought on “Medical Care As We Know It In The US Is Unsustainable.”